Older adults, those aged 60 or above, make important contributions to society as family members, volunteers and as active participants in the workforce. While most have good mental health, many older adults are at risk of developing mental disorders, neurological disorders or substance use problems as well as other health conditions such as diabetes, hearing loss, and osteoarthritis. Furthermore, as people age, they are more likely to experience several conditions at the same time.
The problem
The world’s population is ageing rapidly. Between 2015 and 2050, the proportion of the world’s older adults is estimated to almost double from about 12% to 22%. In absolute terms, this is an expected increase from 900 million to 2 billion people over the age of 60. Older people face special physical and mental health challenges which need to be recognized.
Over 20% of adults aged 60 and over suffer from a mental or neurological disorder (excluding headache disorders) and 6.6% of all disability (disability adjusted life years-DALYs) among people over 60 years is attributed to mental and neurological disorders. These disorders in older people account for 17.4% of Years Lived with Disability (YLDs). The most common mental and neurological disorders in this age group are dementia and depression, which affect approximately 5% and 7% of the world’s older population, respectively. Anxiety disorders affect 3.8% of the older population, substance use problems affect almost 1% and around a quarter of deaths from self-harm are among people aged 60 or above. Substance abuse problems among older people are often overlooked or misdiagnosed.
Mental health problems are under-identified by health-care professionals and older people themselves, and the stigma surrounding these conditions makes people reluctant to seek help.
Risk factors for mental health problems among older adults
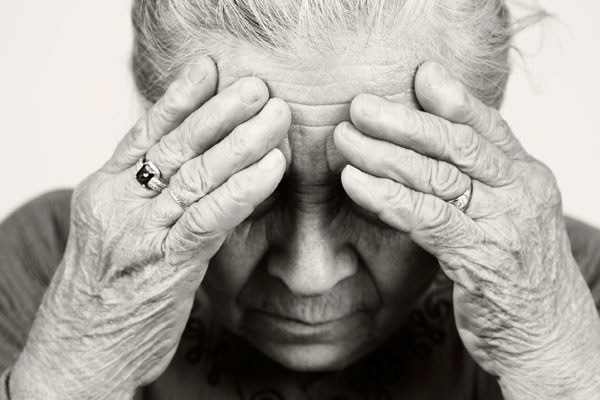
There may be multiple risk factors for mental health problems at any point in life. Older people may experience life stressors common to all people, but also stressors that are more common in later life, like a significant ongoing loss in capacities and a decline in functional ability. For example, older adults may experience reduced mobility, chronic pain, frailty or other health problems, for which they require some form of long-term care. In addition, older people are more likely to experience events such as bereavement, or a drop in socioeconomic status with retirement. All of these stressors can result in isolation, loneliness or psychological distress in older people, for which they may require long-term care.
Mental health has an impact on physical health and vice versa. For example, older adults with physical health conditions such as heart disease have higher rates of depression than those who are healthy. Additionally, untreated depression in an older person with heart disease can negatively affect its outcome.
Older adults are also vulnerable to elder abuse – including physical, verbal, psychological, financial and sexual abuse; abandonment; neglect; and serious losses of dignity and respect. Current evidence suggests that 1 in 6 older people experience elder abuse. Elder abuse can lead not only to physical injuries, but also to serious, sometimes long-lasting psychological consequences, including depression and anxiety.
Dementia and depression among older people as public health issues
Dementia
Dementia is a syndrome, usually of a chronic or progressive nature, in which there is deterioration in memory, thinking, behaviour and the ability to perform everyday activities. It mainly affects older people, although it is not a normal part of ageing.
It is estimated that 50 million people worldwide are living with dementia with nearly 60% living in low- and middle-income countries. The total number of people with dementia is projected to increase to 82 million in 2030 and 152 million in 2050.
There are significant social and economic issues in terms of the direct costs of medical, social and informal care associated with dementia. Moreover, physical, emotional and economic pressures can cause great stress to families and carers. Support is needed from the health, social, financial and legal systems for both people with dementia and their carers.
Depression
Depression can cause great suffering and leads to impaired functioning in daily life. Unipolar depression occurs in 7% of the general older population and it accounts for 5.7% of YLDs among those over 60 years old. Depression is both underdiagnosed and undertreated in primary care settings. Symptoms are often overlooked and untreated because they co-occur with other problems encountered by older adults.
Older people with depressive symptoms have poorer functioning compared to those with chronic medical conditions such as lung disease, hypertension or diabetes. Depression also increases the perception of poor health, the utilization of health care services and costs.
Treatment and care strategies to address mental health needs of older people
It is important to prepare health providers and societies to meet the specific needs of older populations, including:
- training for health professionals in providing care for older people;
- preventing and managing age-associated chronic diseases including mental, neurological and substance use disorders;
- designing sustainable policies on long-term and palliative care; and
- developing age-friendly services and settings.
Health promotion
The mental health of older adults can be improved through promoting Active and Healthy Ageing. Mental health-specific health promotion for older adults involves creating living conditions and environments that support wellbeing and allow people to lead a healthy life. Promoting mental health depends largely on strategies to ensure that older people have the necessary resources to meet their needs, such as:
- providing security and freedom;
- adequate housing through supportive housing policy;
- social support for older people and their caregivers;
- health and social programmes targeted at vulnerable groups such as those who live alone and rural populations or who suffer from a chronic or relapsing mental or physical illness;
- programmes to prevent and deal with elder abuse; and
- community development programmes.
Interventions
Prompt recognition and treatment of mental, neurological and substance use disorders in older adults is essential. Both psychosocial interventions and medicines are recommended.
There is no medication currently available to cure dementia but much can be done to support and improve the lives of people with dementia and their caregivers and families, such as:
- early diagnosis, in order to promote early and optimal management;
- optimizing physical and mental health, functional ability and well-being;
- identifying and treating accompanying physical illness;
- detecting and managing challenging behaviour; and
- providing information and long-term support to carers.
Mental health care in the community
Good general health and social care is important for promoting older people’s health, preventing disease and managing chronic illnesses. Training all health providers in working with issues and disorders related to ageing is therefore important. Effective, community-level primary mental health care for older people is crucial. It is equally important to focus on the long-term care of older adults suffering from mental disorders, as well as to provide caregivers with education, training and support.
An appropriate and supportive legislative environment based on internationally accepted human rights standards is required to ensure the highest quality of services to people with mental illness and their caregivers.
WHO response
WHO supports governments in the goal of strengthening and promoting mental health in older adults and to integrate effective strategies into policies and plans. The Global strategy and action plan on ageing and health was adopted by the World Health Assembly in 2016. One of the objectives of this global strategy is to align the health systems to the needs of older populations, for mental as well as physical health.…